If You Ghosted Your IOP, You’re Not a Failure
Let’s get this out of the way: leaving your intensive outpatient program early doesn’t make you lazy, selfish, or hopeless. It means you’re human—and probably overwhelmed.
Most people who pause or disappear from treatment don’t do it because they don’t care. They do it because their life is on fire in five different directions. Because they’re working two jobs. Because their kid got sick. Because therapy got too real too fast. Because showing up felt like too much.
At Foundations Group Recovery Center in Falmouth, MA, we’ve seen this story before—and we’re not here to shame you for it. We’re here to show you it’s still possible to come back, recalibrate, and make IOP work alongside everything else you carry.
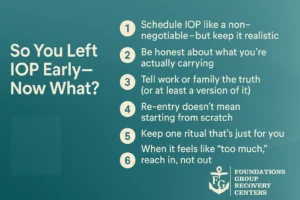
1. Schedule IOP Like a Non-Negotiable—But Keep It Realistic
One of the hardest things about IOP isn’t the therapy. It’s the calendar.
You’re trying to heal and hold down a job, parent your kids, show up for a partner, stay on top of bills, and not crumble in public.
The truth? IOP won’t work if you treat it like an “extra.”
It has to be a non-negotiable, like dialysis or insulin. Not because it’s urgent—but because it’s essential.
That said, a good IOP doesn’t expect you to blow up your life to participate. At Foundations, we offer flexible group times (mornings, evenings, part-time options), so your schedule isn’t the thing that takes you out.
If you’re looking for an intensive outpatient program in Barnstable County, MA or Falmouth, ask about availability that actually fits into your life—not around it.
2. Be Honest About What You’re Actually Carrying
A lot of people walk into IOP trying to be high-functioning.
You want to be the “good client.” You don’t want to take up space. You don’t want to admit that you cried in the car before group or haven’t slept through the night in weeks.
Here’s the truth: your IOP team isn’t judging you. They’re listening for how to help.
When clients ghost, it’s rarely because they don’t want recovery. It’s because they felt like no one saw how heavy their life really was.
Being honest—“I’m tapped out. I feel guilty every time I leave my kids. I hate my job but I can’t quit”—opens the door to real support.
Your therapist can’t change your life’s circumstances, but they can help you carry them differently. You don’t have to pretend everything’s fine while falling apart inside.
3. Tell Work or Family the Truth (or at Least a Version of It)
One of the sneakiest ways burnout creeps in? No one else knows you’re in treatment.
So your boss still expects 110%. Your partner still assumes you’re “just at a doctor appointment.” Your mom still wants help with errands after group.
Telling the people in your life you’re doing mental health treatment three times a week can sound terrifying—but it might also save your energy and your spot in IOP.
You don’t have to give all the details. Try:
- “I’m taking time to work on my mental health and recovery right now. I go to a group three mornings a week.”
- “I’m in a structured program that’s helping me manage stress and get back on track.”
- “I’m doing something for myself that helps me stay grounded.”
Need a letter? Documentation? Help explaining it? We’ve got you.
Letting people know your time has limits isn’t selfish—it’s survival.
4. Re-Entry Doesn’t Mean Starting From Scratch
Here’s something most people don’t realize: coming back to IOP doesn’t mean you’re going backwards.
You’re not starting over. You’re building from where you left off.
Even if you missed a week. Or a month. Even if you relapsed or shut down or ghosted the group chat entirely.
If you came for three sessions and then disappeared, you still learned something. You still noticed something. That part of you that said, “I should probably go back” is worth listening to.
We’ve had clients return after six months and pick up their healing like a thread they never really dropped.
You’re not broken. You’re still in process.
5. Keep One Ritual That’s Just for You
Balancing IOP, work, and family doesn’t just require calendar management—it requires emotional maintenance.
You can be in therapy three times a week and still feel like you’re losing your mind if you don’t have something that belongs just to you.
Pick one thing. Just one.
- A 10-minute walk alone before group.
- A playlist you listen to every time you drive to session.
- A coffee after IOP where you sit in the car and breathe.
- A moment at night when you journal three words—no full sentences required.
This isn’t homework. It’s a lifeline. Recovery isn’t just about what happens in group—it’s about remembering you’re a person, not a task list.
6. When It Feels Like “Too Much,” Reach In, Not Out
There will be a day (maybe soon) when it all feels like too much.
You’ll think about skipping group. You’ll convince yourself no one will notice. You’ll scroll instead of texting your counselor. You’ll say, “I’ll just take a break for now.”
Before you disconnect, ask yourself: What would happen if I reached in instead of out?
Text the group leader. Call the front desk. Say, “I don’t think I can come today, but I don’t want to ghost.” That one sentence can change everything.
You’re allowed to struggle in IOP. You’re allowed to come in messy. You’re allowed to take a breath and say, “This week was hard.”
You don’t have to be perfect. You just have to stay connected.
Why Our IOP Works for People with Real Lives
Foundations Group Recovery Center in Mashpee, MA, offers an intensive outpatient program that’s not just clinical—it’s real-life capable.
We designed it for people who:
- Have jobs, kids, or caregiving responsibilities
- Can’t afford to disappear for 30+ days
- Need help but also need to stay in motion
- Want support without shame
- Might have tried therapy before and still felt stuck
You’ll get trauma-informed care, real tools for stress and triggers, and a community of people who get it—not because they read a book, but because they’ve lived it too.
We don’t expect you to be healed when you arrive. We just ask that you show up—however you are.
FAQ: IOP Logistics, Emotions, and Re-Entry
Is it okay to come back if I ghosted before?
Yes. We mean that. No judgment. No lectures. Just help picking up where you left off.
What if I have a weird schedule or multiple jobs?
Talk to us. We offer flexible sessions and will do our best to build something that works for you.
Can I do IOP and still care for my kids?
Yes. We work with many parents. Let us know what support you need to make it possible.
Do I have to talk in group if I come back?
Nope. You can sit quietly. You can cry. You can speak when you’re ready. There’s no pressure to perform.
Will I be judged if I relapsed or quit last time?
Not here. We see re-entry as a sign of strength. Coming back is part of the process—not proof of failure.
Call (844)763-4966 or visit our intensive outpatient program page to learn more about our IOP in Mashpee, MA—and how it can flex around your life.